WHY MENTAL HEALTH MATTERS - with Prof. Edward Callus, CHD Clinical Psychologist
Hospitalizations and medical interventions leave lasting marks on children with CHD, far beyond physical scars. This post explores the importance of mental health support, resilience, and family involvement in shaping a better quality of life for our young warriors.

The first session after my 6-year-old daughter's cardiac catheterization, her psychotherapist suggested we do some role play. I had shared beforehand that I noticed heightened anxiety and signs of PTSD in Emanuela's behavior. She had become shy in ways she hadn't been before. Facing the unknown triggered full-blown panic attacks. She was more cuddly, more clingy, more frustrated. Her whole way of being was "more" than usual. So, we role-played.
We took a doctor's kit play box off the therapist's shelf. Emanuela was hesitant at first, but we gently convinced her it could be fun. I became the patient, and Emanuela took on the role of doctor. Initially reluctant, she quickly embraced the game. She grabbed the toy knife and went straight for my neck. Pretending to cut it, she laughed loudly and said, "Here, I cut your head off!"
It wasn't laughter from joy or amusement. I know my child well. She laughed to mask discomfort. The smile on her face was a shield. In truth, she felt insecure, awkward, maybe shy, and surely - angry. She must have been angry at the whole world. Me included.
Emanuela has been poked, cut, wired, tubed, and stripped of her choices, decisions, and ultimately her dignity more times in her short life than most people endure in a lifetime. Her world of multiple open-heart and abdominal surgeries, countless tests, and procedures is a violent one. And I am the one guiding her through it. It makes me angry. How could it not fill her with rage? The difference is, I understand my anger, and I know she is allowed to be furious, too. But I hadn't considered that she might not realize she can feel like cutting my head or anyone else's off. Of course, while she is allowed to feel that way, she cannot act on it. Teaching this distinction is where parental guidance and child play therapy come in.
Why? You ask.
Children born with a congenital heart defect (CHD) experience twice as much psychopathology as their healthy peers. Challenges like social difficulties, delinquent behavior, anxiety, depression, or withdrawal can manifest even a decade after the surgery.
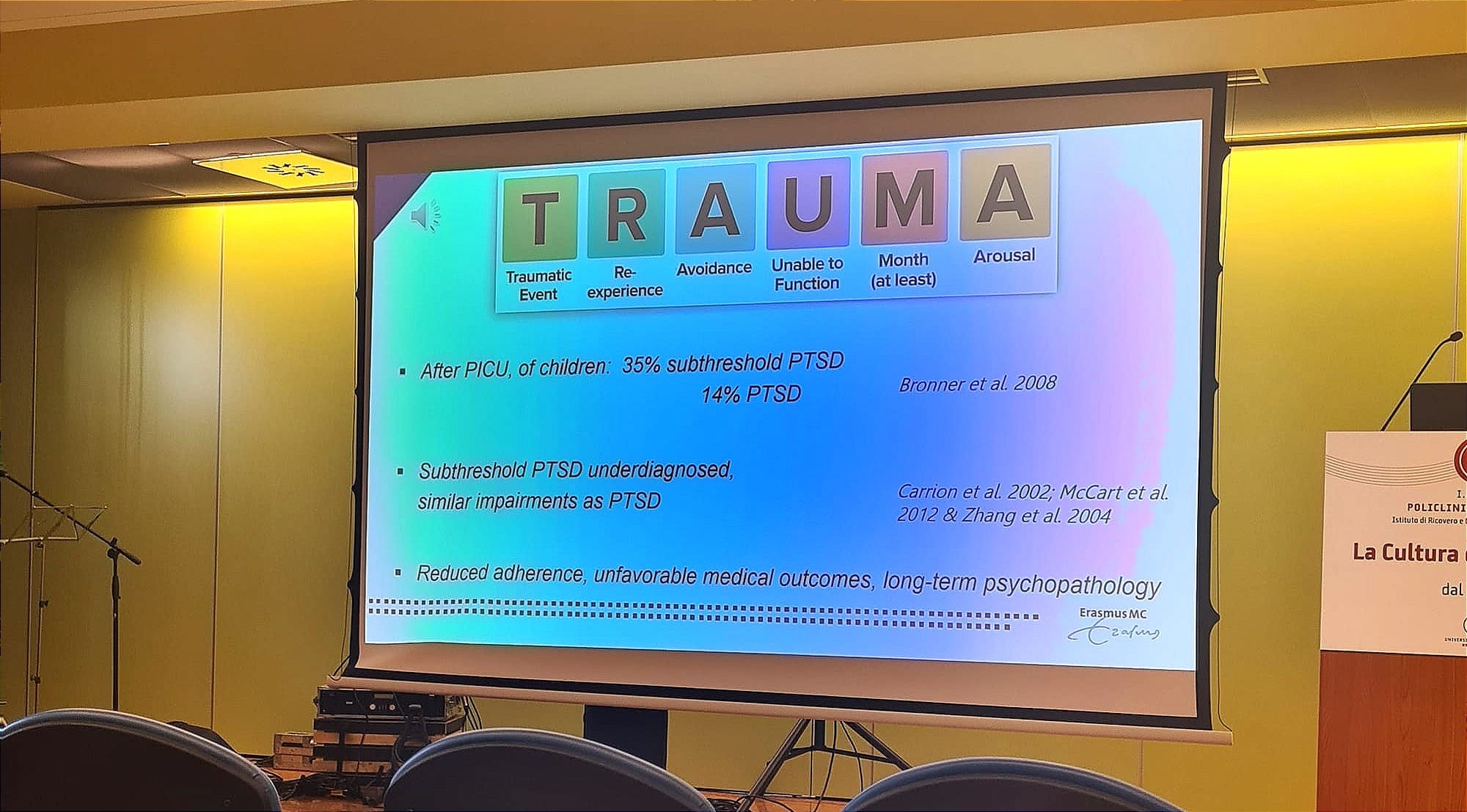
Prof. Dr. Elisabeth Utens highlighted this at the neurodevelopment and psychosocial care working group meeting of the Association for European Paediatric and Congenital Cardiology in Milan, Italy. Her research focuses on the CHD population. One of her findings shows that the higher number of hospitalizations correlates with greater psychopathology within the first 30 years of life. The quality of life for her study's patients only started improving in adulthood as they learned to cope.
So, I guess it's encouraging that these issues lessen with age. But what about our children?

Prof. Edward Callus recently reminded me of Prof. Utens' presentation, which made it clear that anxiety-related trauma in hospitals is one of the biggest challenges.
Many children experience anxiety before surgery, and hospital procedures can lead to symptoms of trauma or stress after discharge. Early identification of at-risk children is critical for preventing long-term effects. Collaboration among psychologists, nurses, and physicians is vital to creating a trauma-free hospital environment.
(Prof. Edward Callus, Clinical Psychologist - Italy)
As medical advancements improve outcomes for children with CHD, the focus has shifted from survival to quality of life. More than 90% of children with CHD now survive into adulthood, making it crucial to incorporate physical, cognitive, and social aspects into comprehensive, multidisciplinary care.
Why Mental Health Matters
Multiple surgeries, frequent interventions, and long hospitalizations are undoubtedly linked to possible cognitive delays, such as difficulties in learning, understanding, and processing. White matter* damage during surgery is a risk that can impair memory and executive functions, like planning, organizing, prioritizing, and task execution. Emotional and behavioral challenges - anxiety, depression, ADHD-like symptoms, and social withdrawal - are all more common in children with CHD than their healthy peers.
Studies suggest that differences in brain development, even during the prenatal stage, can affect oxygen flow. This may result in motor skill challenges or coordination difficulties, often linked to white matter changes. Early identification and individualized care plans are crucial for helping children achieve their full potential academically and socially.
(Prof. Edward Callus, Clinical Psychologist - Italy)

Considering all that's been said, it becomes evident that holistic care is the only viable way forward. Neurodevelopmental, emotional, and psychological support for both patients and families must be integral to our children's routine medical care. To answer the title's question directly: Mental health matters because addressing developmental and psychological challenges early on provides children living with half a heart, and other forms of CHD, with improved long-term outcomes and a significantly enhanced quality of life.
Today, we understand that specific learning difficulties, once overlooked or undiagnosed, are not only prevalent but critically relevant during childhood. Early recognition and intervention are key. When problems are identified and addressed promptly, children receive the support they need to thrive, often performing better and catching up with their peers more quickly than they would without intervention.
(Prof. Edward Callus, Clinical Psychologist - Italy)
- MOTOR DELAYS: late crawling, difficulty walking, drawing, threading beads and manipulating small objects, etc.
- BEHAVIORAL CHALLENGES: emotional outbursts, withdrawal, anxiety, ADHD, etc.
- COGNITIVE ISSUES: memory, planning, task management, etc.
- LEARNING STRUGGLES: language development, processing speed, etc.
Prof. Callus and his community of experts emphasize the importance of therapies like Cognitive Behavioral Therapy (CBT) and Eye Movement Desensitization and Reprocessing (EMDR) for anxiety and trauma management.
These types of treatment must be integrated into hospital settings, and supported by multidisciplinary teams in order to achieve results.
(Prof. Edward Callus, Clinical Psychologist - Italy)
And How are You, dear Mom?
Children, however, cannot be removed from the family equation. Surgical interventions, medical procedures, and hospitalizations impact the entire family. Prof. Callus highlights the need for developmental assessments that include families, as addressing the broader family dynamic is critical to improving outcomes for children.
Different socioeconomic backgrounds bring unique mental health challenges and cognitive outcomes, requiring tailored support systems. Peer support groups - offering emotional connection, information exchange, and enhanced coping mechanisms - are invaluable. Families who engage in self-help or peer support groups often demonstrate stronger emotional resilience, which positively influences their ability to navigate challenges.
(Prof. Edward Callus, Clinical Psychologist - Italy)
Parents' ability to manage their emotions plays a pivotal role in supporting their children. When families are emotionally resilient, children benefit directly through better emotional stability and mental health.
As I've learned from the Milan conference I mentioned earlier and from webinars led by community leaders at the European Congenital Heart Disease Organisation, fostering healthy emotional expression and creating robust support networks are key to maintaining a stable family environment.
So, I let Emanuela play at cutting my head off.
Later that day, I asked her why she did it. Her response was simple. She wanted to look into me and check if my heart was working well. But, she added, I shouldn't worry - she made sure to sew my head back on. And that was it. No fuss.
This moment stayed with me. It reminded me of how children process their emotions in unexpected ways. To support Emanuela, I've started a habit of reminding her that it's okay to be angry, even at me. "Mommy's not perfect," I tell her. "Mommy, you're the best," she always replies. We hug, and we leave the rest for another play session at her therapist's office.
*WHITE MATTER = A network of nerve fibers in the brain allowing communication between different areas. Decreased blood flow and nutrients to the white matter can cause damage to these nerve fibers, and damage can cause memory issues, balance problems, and mood changes.
(Cleveland Clinic, White Matter Disease)
Medical Disclaimer
This article is for informational or educational purposes only. It does not substitute professional medical advice, diagnosis or treatment. Always seek the advice of a physician or other qualified health provider.

