TACHYCARDIA - From Panic to Peace

Irregular heartbeat (arrhythmia) kept our baby girl on the edge of life and death after her first open-heart surgery. During those first few months of her life, tachycardia would tire her heart so badly that she would be rushed to the Intensive Care Unit (ICU) and put on a ventilator every time. That would give her time to rest, and her heart to regain strength. She became a bit stronger to handle it after the second open-heart surgery, at the age of four months.
TACHYCARDIAS, or fast heart rhythms, are often the result of misfiring electrical signals in the upper or lower heart chambers, which drown out signals from the sinus node (a small area of tissue in the right upper chamber of the heart). This may happen due to a “hot spot” in the heart that is beating too rapidly or abnormal additional electrical pathways within the heart that cause the electrical signal to race around a loop.
(Children's Hospital of Philadelphia)
As much as we were getting ready during the months before her birth for everything ahead with her initial diagnosis, heart arrhythmias were something no one could have predicted. And as much as we were knowledgeable about a single ventricle heart at the time, when they told us about tachycardia, a racing heart, we were numbed. What's that now?! By that point, I was already getting fatigued from all the researching and reading and learning about everything new that was happening to her almost daily, and the idea of adding more things to the study and worry list was overwhelming.
There are different types of tachycardia. SVT is the one that caused our baby girl's heart to beat too fast...
Recognizing Tachycardia
Over time, I've learned enough about it to feel confident recognizing when it fires up my baby's heart, and comfortable handling it.
While an ECG is the most reliable test to detect an irregular heartbeat, a parent can learn to recognize the symptoms.
What I did, as soon as I noticed Emanuela behaving unusually, was put my hand on her chest and stand still for a moment. When the heart beats so fast and strong, as hers did, the hand on the chest is enough to feel it.
When in doubt, I would try counting the heartbeats out loud. In a state of tachycardia, that is impossible without a tongue getting twisted and the head being unable to follow.
Finally, if I were still uncertain, I always had a stethoscope at hand, while being mindful that the point was not for me to diagnose it, but to recognize when medical help was required.
Rushing from the cardiac ward to the ICU of the paediatric hospital was eventually replaced by us driving down the highway, with all four blinkers on, hoping everyone else on the road would understand we were having an emergency.
Waiting It Out vs. Visiting the ER
One summer I walked with her along the beach when she suddenly started crying at the pier. We were not so close to our things, and she was refusing to walk. When I kneeled down to try and talk to her, I touched her chest and immediately felt her heart pounding. I started running, trying not to sprain my ankle on a pebble beach, with her in my hands, towards my mom who immediately knew something was wrong. We left all our things there and continued straight to the car and home, where we had her medicine. I remember calling her doctor, a specialist in heart arrhythmias, for a consult. At that time, I was uncertain and indecisive between waiting it out and visiting the ER. But seeing my mom pale and frightened for her granddaughter, I thought a visit to the hospital might at least give her some peace of mind. By the time we parked the car, tachycardia had stopped. (It took a bit longer for Grandma's nerves to calm.)

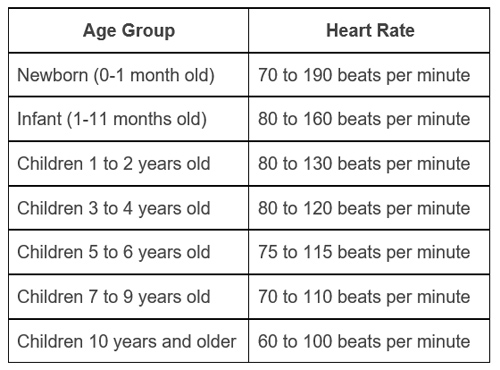
Much like that summer day, Emanuela's heart had us cut short both the New Year's Eve of 2019 transitioning into 2020 and her second birthday, three weeks later. Having tachycardia meant her heart rate jumped from a normal range of 80 - 130 beats per minute to anywhere between 180 and 230. That made her face lose colour, her limbs lose strength, and her body lost somewhere between being awake and asleep.
With her having a tachycardia episode quite often, we decided to invest in our own ECG device. That made it very easy to manage her racing heart.
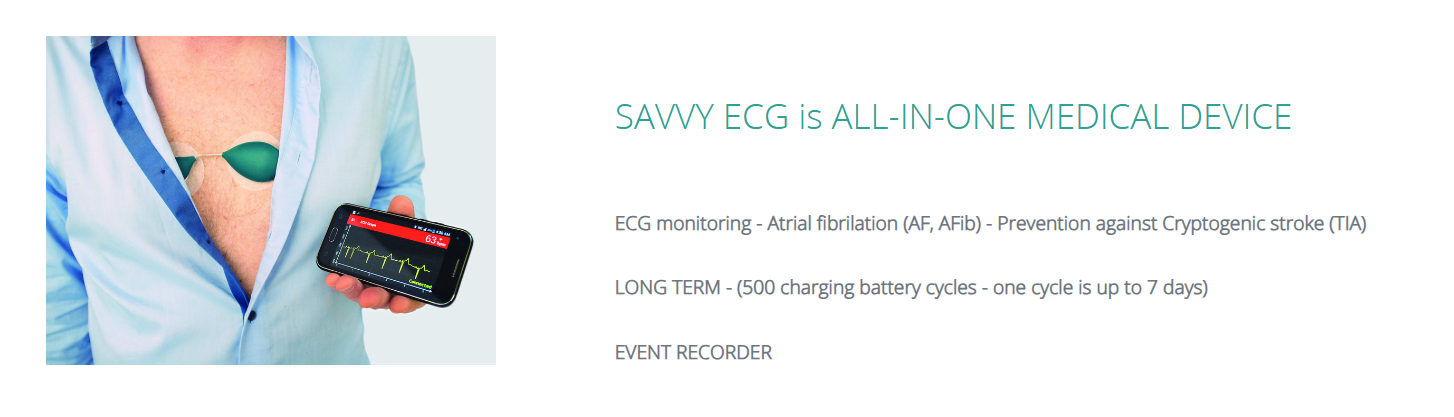
As soon as I saw her behaving strangely, I would do my routine. Once I confirmed she might be tachycardic, I would glue the sticker electrodes to her chest, tune my mobile app to it, and follow what was going on with her heart. It would make me hopeful when numbers would show her heart slowing down, but often, I would not even finish my thought and it would pick up the speed again. That was the cue - we had to go to the hospital.
Stopping Tachycardia
It took time to get used to her looking the way she did when her heart exhausted her and be rational enough to first wait it out, and only then, if needed, to drive her to the ER within the speed limit. I have to be honest though... I do not remember us ever waiting it out longer than an hour. (Not sure that was scientifically "rational enough", but it was all I could muster.)
When she was younger, she was given medication to manage her racing heart. However, the domestic dose and oral intake did not always work. When tachycardia persisted, she required intravenous administration of medication in a hospital setting.
Little tricks like putting an ice cube on a neck or a cheek or invoking a gag reflex by putting a spoon below the tongue... those and other vagal maneuvers never worked for us.
As soon as she was a bit bigger and stronger, around the age of two, her cardiologist suggested turning her upside down. That actually helped once or twice, when she was not screaming and crying and making it all together impossible to perform.
These are mostly meant for adults, but some of them can be tried out with children.
- Bearing down like having a bowel movement
- Holding breath and submerging the face in water
- Neck massage
- Gag reflex
- Coughing
- Handstand for 30 seconds
- Applied abdominal pressure
(Cleveland Clinic)
When we were first introduced to the world of heart arrhythmias, we were told that babies can outgrow it within the first year of their lives. I cannot find words to express the depth of our hope. To have one thing come and go - "easily".
That didn't happen.
Depending on your child's age and the severity and frequency of symptoms, the cardiologist may recommend a catheter ablation procedure to permanently eliminate Supraventricular Tachycardia (SVT). During ablation, several large IVs (small plastic tubes) are placed in the main blood vessels in the legs. Then, catheters (thin tubes) are advanced up through the veins and into the heart. Electrical signals from the catheters help locate the extra electrical connection, which can then be destroyed and eliminated. The procedure takes several hours, and most children can go home on the same day. After successful treatment with ablation, the child should not experience any SVT episodes.
(Children's Hospital of Philadelphia)

Since October 2020, our little girl has been free of tachycardia. It took two cardiac ablation procedures and a temporary pacemaker to get us there (more about that is in a post Unexpected turns: from Heart Arrhythmias to Pacemaker Placement). However, years later, I still catch myself putting a hand on her chest. It became a habit, but feeling her heartbeat is also a reassurance and a moment for gratefulness.
Symptoms:
- Sudden crying
- Lack of energy
- Becoming pale
- Loose body / falling asleep
(Adults report chest pain, shortness of breath, and dizziness.)
Confirmation Tools:
- Hand on the chest
- Counting heartbeats
- Stethoscope
- ECG
Ways to Stop it:
- Waiting it out
- Ice cube put on the neck or the cheek
- Invoking gag reflex
- Turning upside down
- Medication
- Cardiac ablation
Medical Disclaimer
This article is for informational or educational purposes only. It does not substitute professional medical advice, diagnosis or treatment. Always seek the advice of a physician or other qualified health provider.