Dear Diary... is this PTSD?
I was told I am brave and that our story is inspiring so many times that it does not leave any room to think otherwise. Hence, I do not dare saying just how scared I can be and how dark my thoughts can go. By saying how anxious I can get and how vivid my fearful imagination can be, I could risk stopping being brave and inspiring. Not to you. To myself.
Following the exposure to a traumatic incident, it is quite common to replay the event in your mind, often as nightmares and flashbacks. This is how our minds make sense of what was going on at the time. Following these challenging situations, it is also common and understandable to feel anxious, angry, guilty, and sad. We may experience difficulty sleeping and continue to feel on guard after the situation is over. Often we try to avoid reminders of the trauma to block out thinking about it.
All of these signs are a normal response to an unusually difficult situation. Usually, they will fade in the days and weeks after the event. Sometimes they persist and develop into a more serious anxiety disorder known as posttraumatic stress disorder (PTSD).
(Healing Heart and Minds, A Holistic Approach to Coping Well With Congenital Heart Disease, by Tracy Livecchi, LCSW and Liza Morton, PhD, p. 50-51)

There is a part of the highway that always reminds me of all the times when we were racing with our daughter to the ER. Needless to say that the highway leads to many places, not just to the hospital. So, basically, almost wherever we go, there's the flashback.
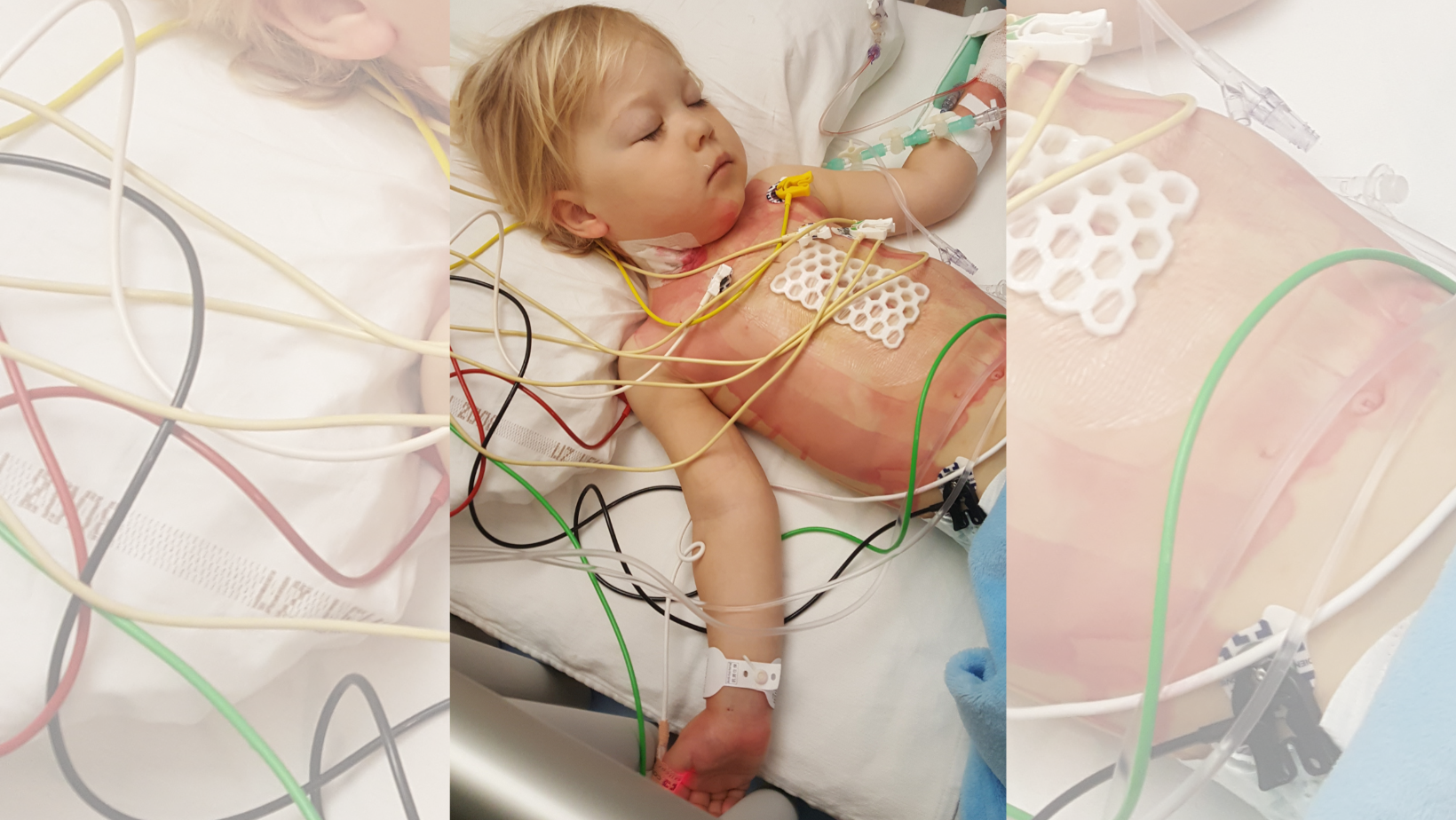
The memories of her body slowing down in the back-seat, while her heart raced at 230 beats per minute; her being held upright only by the chair's straps as her back and limbs lost all their strength and became relaxed, soft, motionless; her face losing colour to a point where pale doesn't even describe it... three years later - I can still see her that way.

As for myself, I don't remember being in a state of panic. I remember staying focused. Her heart would go into a tachycardia*, and I would start a crisis management. I knew what needed to be done. I felt trained for those moments. There was fear, but it did not take over like the anxiety does now, sometimes.
For example, when I look at pictures from that time, there is a limit of how many I can handle. My body reacts, for example, to the smell of the Intensive Care Unit where I have friends working and that I (would) like to visit.
- irritability or anger
- nightmares or disturbing dreams of the traumatic event
- tearfulness
- anxiety
- returning, upsetting memories about the event
- insomnia
- having a startle response, for instance jumping when you hear a loud noise or siren
- going out of your way to avoid any exposure to the hospital or your care team
- inability to concentrate
(Healing Heart and Minds, A Holistic Approach to Coping Well With Congenital Heart Disease, by Tracy Livecchi, LCSW and Liza Morton, PhD, p. 52-53)
We always wanted her doctors to tell us about the worst case scenarios, all possible outcomes; we wanted to know statistics, expected and less probable side effects and consequences; we wanted to know the survival rates. We like to believe that it is what keeps us being real. We are not fooling ourselves. She lives on borrowed time. And that uncertainty makes me feel on guard.
I was for far too long in a fight or flight mode; still often am. And the notion of my daughter going through the same roller-coaster of feelings as she will be growing up and becoming more conscious, makes me sad.

Writing this, I am deeply aware that none of it (or very little) should be about me. It is her fight; her disability. She is the one that had night terrors and (will) have who knows what kind of nightmares. I only had a few.
She is the one wearing the scars. For life.
Seeing her thrive and do something that I know just how long it took us to get to, makes me tearful. Like her jumping on a trampoline, when I know what it took to have her make her first step.
I could barely hold myself together at her school's end of year show, seeing her dance and sing on a stage with her peers, knowing how long we kept her away from children to avoid her getting sick; and being aware how easily she might not have been with us at all. She survived against all odds.
At the same time, I can feel guilty for not being grateful for it all the time. I feel angry at myself when I raise my voice and when I am being harsh on her; when I am being a parent. As if having her alive is not enough.
Today, our Emanuela is five years old. I can only speak of the way her CHD affects me, and hope that one day she will find a voice of her own. Since a congenital heart disease is a life-long condition, it is impossible to avoid reminders in order not to think about the trauma. It would be like not thinking about life. If nothing else, the scars make sure the memory stays.
11-21% of adults with a CHD had a diagnosis of PTSD compared to 3.5% in the general population
(Healing Heart and Minds, A Holistic Approach to Coping Well With Congenital Heart Disease, by Tracy Livecchi, LCSW and Liza Morton, PhD, p. 51)
So...
Dear Mom... is this PTSD? I don't know. But according to psychologists and authors T. Livecchi and L. Morton, a quarter of mothers and fathers will be experiencing acute PTSD 6 months after their child has undergone cardiac surgery.
It is perhaps not surprising to find this increased risk of developing PTSD in the CHC population, considering we are often exposed to the perfect storm of risk factors such as repeated, often unexpected, health crisis and interventions while juggling additional life stressors often without adequate social support, which may result in what has been termed "cardiac disease-induced PTSD" (CDI-PTSD).
(Healing Heart and Minds, A Holistic Approach to Coping Well With Congenital Heart Disease, by Tracy Livecchi, LCSW and Liza Morton, PhD, p. 52)
CHD is a life-long condition. It is inevitable that all these feelings become an intense life-long companion that can be hostile or friendly. Learning to accept them is a skill in itself. I say - keep breathing.
One breath in. One breath out. And repeat.
To carry the load is brave. To keep going is inspiring.
*TACHYCARDIA is a heart rhythm disorder with heartbeats faster than usual.
Medical Disclaimer
This article is for informational or educational purposes only. It does not substitute professional medical advice, diagnosis or treatment. Always seek the advice of a physician or other qualified health provider.