After the heart is fixed...

One of the first things I have learned at the beginning of this journey of ours, I remember, was that fixing a single ventricle heart is palliative. Palliative, I thought, as in sitting next to a terminally ill person, holding hands and waiting to die. But it turned out that that was not the right picture in my mind.
96% of babies born with a heart defect will live to celebrate their 10th birthday, and around 92% will reach the age of 20.
(MUDr. Petr Hecht, paediatric cardiologist at the University hospital Motol, Prague, Czech Republic)
According to the statistics that Dr. Petr Hecht presented at the meeting of single ventricle patients and their families living in the Czech Republic in January, 2023, 6.16 babies per 1000 are born with a heart defect. Among those, 3% have a single ventricle heart. In the Czech Republic, that is 20 kids each year. World-wide, however, there are roughly 50.000 to 80.000 people living with half a heart.
While, unfortunately, 25% of babies born with a critical heart defect will not live to celebrate their first birthday, around 85 - 90% of children born with a CHD do make it into adulthood. In 1960 that was the case with only 20% of heart children.
Therefore, with a bit of regular maintenance, a full life is very much possible with half a heart.
How full can a life be?
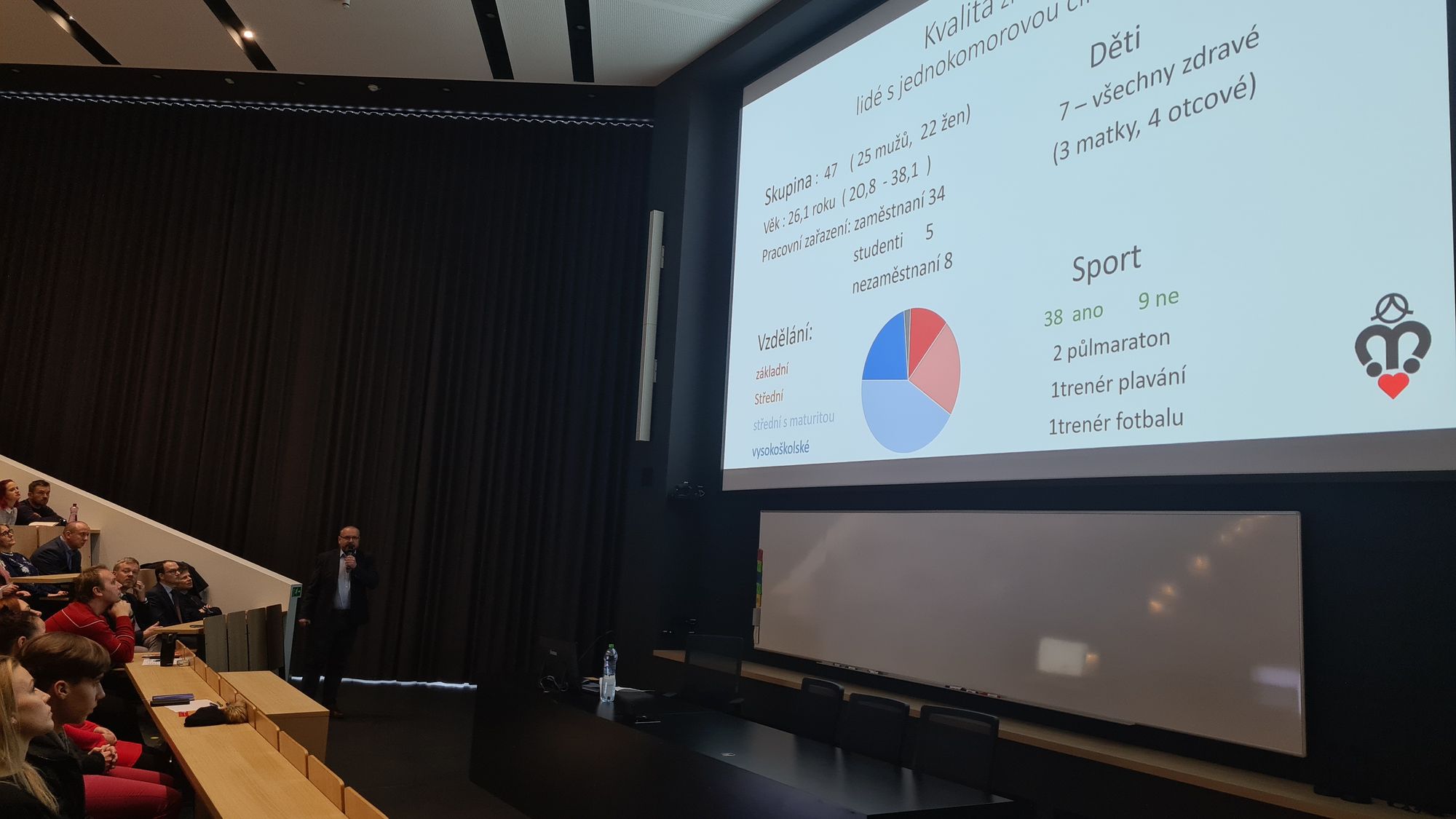
One more thing Dr. Petr Hecht presented at the above mentioned meeting was tangible data they gathered on quality of life with half a heart.
They took a sample of 47 adults with a single ventricle heart, between the age of 20 and 38. There were 25 men in a group and 22 women.
Five of them were students, 8 were unemployed, but the majority had a source of income.
Around a quarter of the group had a university degree and around one third successfully finished high school.
Maybe most importantly - not only did 38 patients do sports, but two of them ran half-marathon, one is a swimming coach and another one a football coach.
Personally, I was mind-blown to see seven of them, three moms and four dads, having children of their own.
Maintaining a full life
Once the heart is as fixed as it can be, the gears switch from life-saving to prevention and maintenance.
Protocol for stable cases requires a check-up every two years. That includes clinical examination, ECG, echocardiography, holter (24h ECG) and a full blood work. Ergometry is done once the child reaches a height of 130cm. As of the age of 12, we add MRI of the heart which is then repeated every 4 years.
In the case of an unstable circulation, check-ups are needed more often.
(MUDr. Petr Hecht, paediatric cardiologist at the University hospital Motol, Prague, Czech Republic)
Ergometry is a procedure that determines the influence of physical activity on heart work. Basically, it is a stress test that gives information about the performance of the heart, ECG changes, changes of the blood oxygenation and values of the blood pressure when the heart is under exertion (heart load test).
Because echocardiography does not show every single detail, MRI of the heart is needed to get the exact information about the sizes and volumes of the heart compartments; it measures valve leakage and ventricular function; displays what is inaccessible, like pulmonary nodules; provides information about changes in the wall of the heart compartments; displays the coronary arteries supplying the heart. The advantage of the MRI is also that it can be repeated and is done without radiation.
The aim of a long-term follow-up is prevention and treatment of later complications like ventricle failure, valves stop closing, formation of blood clots, developing collaterals (vascular connections between the pulmonary artery and the heart) and heart rhythm disorders.
(MUDr. Petr Hecht, paediatric cardiologist at the University hospital Motol, Prague, Czech Republic)
The second first thing I have learned at the beginning of this journey of ours is that with the heart, it is almost never only about the heart.
HEPATIC (liver) - function impairment or ligament remodeling
ABDOMINAL - loss of protein in the intestine
PULMONARY - formation of mucus plugs in the bronchi
HEMATOLOGY - changes in the function of the blood
RENAL (kidney) - decrease in filtration capabilities or protein loss