Single ventricle heart - how to fix it? (WITH VIDEOS)
It takes three open heart surgeries to fix a single ventricle heart. The first two surgeries have to be done within the first few weeks and months of a baby's life, while the third one is usually performed some time between the age of 2 and 6 years.
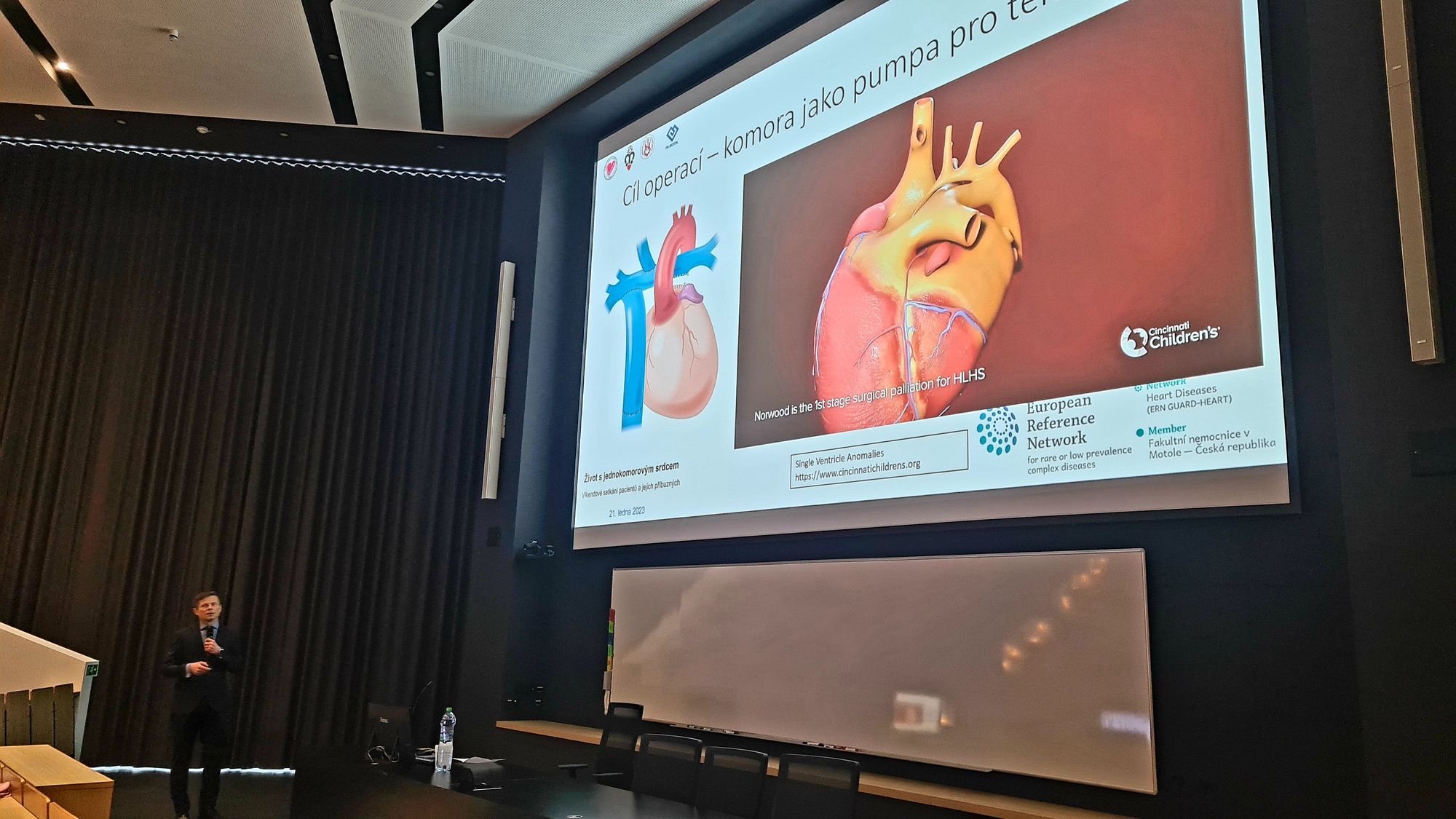
I. NORWOOD OPERATION
Babies born with a single ventricle heart will undergo the first surgery, named Norwood, in the first few days or weeks after birth, when the heart is the size of a walnut.
This procedure, as shown in the animation, takes the one good ventricle, the right ventricle, and changes the plumbing so it now pumps blood to the body, rather than to the lungs. To make sure the lungs also get blood flow, a new connection is added.
The Norwood surgery is one of the most complex and high risk procedures in the staged reconstruction surgeries.
Current survival rate is 75 percent or better.
(Cincinnati Children's)
The recovery period in the hospital following the Norwood operation is often long. It can last from a few weeks to months and thus lead straight into the second stage of fixing a single ventricle heart.
(Wikipedia)
II. GLENN REPAIR
The second stage, named Glenn procedure, will usually take around three hours to complete on a baby between four and six months old.
This procedure changes how blood flow gets to the lungs. A part of what has been done in a Norwood operation is now taken down. The Superior Vena Cava, the vein that collects the blood returning from the upper part of the body, is then connected directly to the pulmonary artery, achieving a passive blood flow to the lungs. The blood returning from the lower part of the body (the inferior vena cava) still returns to the right atrium and ultimately gets pumped out to the body.
During these repairs, we often use patches that are from different materials, such as donated human tissue or from animals, which is specially processed. Or, we insert a Gore-Tex patch. Gore-Tex is a very good material because it remains soft, it does not deform, it holds the shape. That is the same Gore-Tex as is used for clothes. Usually, we use it when we expect growth, like with newborns.
Both these surgeries are relatively complicated. There can be variations of procedures, depending on the anatomy of a defect of the heart.
(MUDr. Rudolf Poruban, congenital cardiac surgeon at the University hospital Motol, Prague, Czech Republic)
However, if all goes well, the expected recovery after the Glenn procedure is between one and two weeks.
(Wikipedia)
III. FONTAN OPERATION
The final of the three steps to fix a single ventricle heart is the Fontan procedure.
The goal is now for all the venous blood returning from the body to go through the lungs first, before returning to the heart to be pumped back out via the single ventricle. This involves connecting the inferior vena cava to the pulmonary artery via a tube graft. This can be done in a few different ways, but is illustrated in the video made by Digital MediaLab team at Cincinnati Children’s with what is called an “extracardiac Fontan” and also shows the addition of a “fenestration.”
Dr. Guillermo Kreutzer from Buenos Aires, Argentina (b. 1934) without any knowledge of Fontan's experience performed a similar procedure in July, 1971 without placing a valve in the Inferior Vena Cava inlet and introducing the concept of "fenestration" leaving a small atrial septal defect to serve as a pop-off valve for the circulation.
(Wikipedia)
(Summarized from Cincinnati Children's Hospital web pages and YouTube videos.)