BASAL STIMULATION - A Parent's Role in Care
Basal stimulation is a simple yet powerful way to support critically ill children. Through my experience with my daughter, I share how small actions can make a big difference in a child's healing, as well as the well-being of the family, and why parental involvement is essential.

"Do you want to touch her?" asked Katka as my husband and I sat helplessly by our daughter's crib. We didn't know where to look, what to say, or how to sit.
When we first met, she was "nurse Katka" to me, but today, she's like family. Our friendship was born from her kindness.
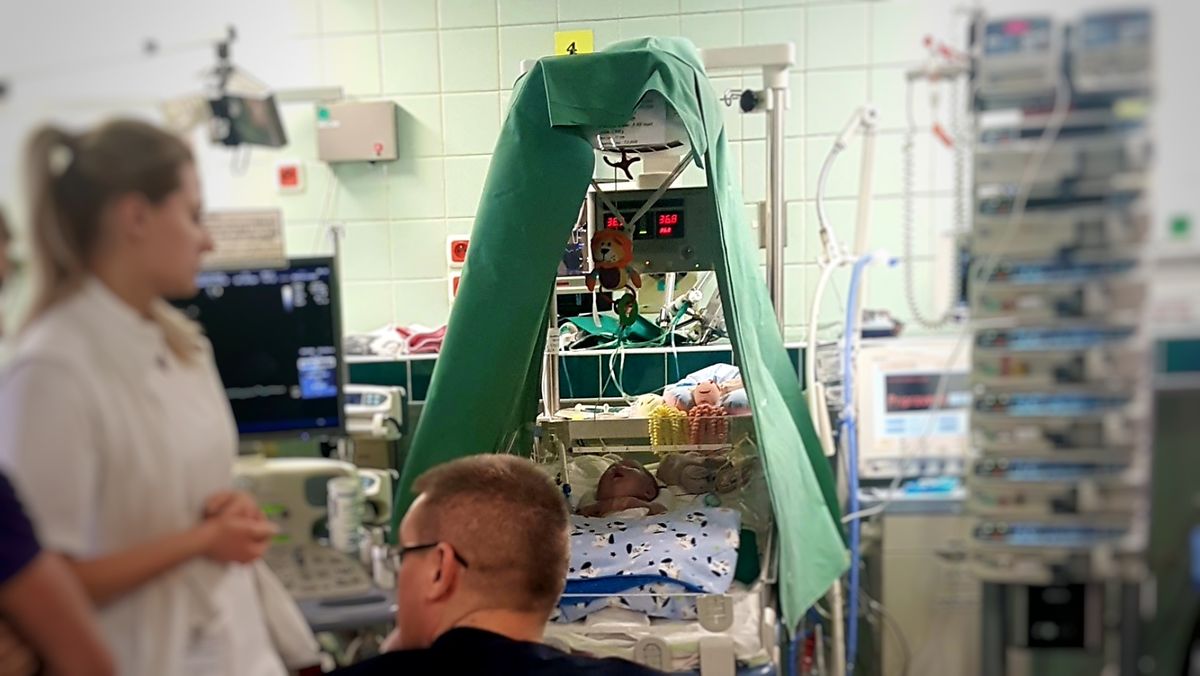
In front of us lay our three-week-old baby, Emanuela, heavily sedated, her tiny heart visibly beating through an open chest wound covered by a transparent surgical patch. Tubes and wires covered her body, connecting her to life support (extracorporeal membrane oxygenation / ECMO). I wondered how so much artificial support could fit on such a tiny being.
Monitors and IV medication dispensers, stacked around us, beeped at regular intervals, reporting every deviation from standard measurements, every finished dose of life-saving drugs. We were in the Intensive Care Unit (ICU) of the Children's Cardiac Center in Bratislava, Slovakia.

A Fragile Touch
"Can we?" I asked, surprised. Now, I wonder why it felt surprising. Did I think I might break my baby? Was I afraid a touch would hurt her? Intimidated by it all, I was terrified of doing something irreversible - like pulling on a tube or disconnecting a wire.
I'd like to say my mind raced with these questions, but in truth, I was numb. All these fears blended into a single, overwhelming feeling. While I wanted to shield my baby from the horrors in front of me, I was frozen in place. She looked so fragile, I barely dared to breathe.
Katka showed me the way. With a smile - kind, yet confident. Professional. Reassuring.
That was all the encouragement I needed. I placed my forefinger on Emanuela's hand and, as gently as possible, stroked from her wrist down to her tiny knuckles, tracing over each of her little baby fingers. I didn't know it then, but that was my first glimpse into the concept of basal stimulation.

Basal Stimulation
The foundations of basal stimulation were developed in the 1970s by German special education teacher Andreas Fröhlich, who worked with children with severe multiple disabilities in a rehabilitation center.
Today, more than fifty years later, basal stimulation remains a recognized nursing and therapeutic approach for people of all ages, from premature infants to critically ill patients and those in end-of-life care. It focuses on sensorimotor and cognitive development, creating communication channels between family members or caregivers and those who cannot express themselves verbally.
In 2001, the International Association for the Promotion of Basal Stimulation was founded to further its practice. Their guiding principle in shaping a world in which everyone has the chance to receive the care and support they need and deserve is clear: Together for a dignified life despite the need for care.
The International Association for the Promotion of Basale Stimulation
The association has regional groups in several countries, including the Czech Republic, where the Institute of Basal Stimulation operates.

The Czech Institute cooperates closely with neighboring Slovakia, where our Emanuela was born. Dr. Ľubica Kováčiková, the chief of the ICU at the Children's Cardiac Center - our first "hospital home" - was the first in the country to implement the concept of basal stimulation.
Basal stimulation has been widely adopted at the Children's Cardiac Centre in the care of children and adults with heart disease. It is used in pediatric cardiology and cardiac surgery departments, as well as in intensive care units, where critically ill children are hospitalized.
(Doc. MUDr. Ľubica Kováčiková, PhD., Chief of Department of Anaesthesia and Intensive Care Medicine, National Institute of Heart and Blood Diseases, Children's Cardiac Center, Bratislava, Slovakia)
Basal stimulation stands out in traditional healthcare because it focuses on the body with deep empathy.
Children in the ICU, especially after cardiac surgery, endure significant physical distress - pain from medical procedures like blood sampling, intubation, bandage changes, and drain removal. Pain is not just a sensation; it's a physical, cognitive, and emotional experience. The goal of basal stimulation is to provide not only rehabilitative care but also compassionate care for the body. By engaging the skin and muscles - such as through gentle baths - we help children develop positive body awareness. Neuroscientific studies confirm the crucial role of these experiences in a child's overall development. Basal stimulation impacts not only sensorimotor functions but also psychosocial and cognitive growth.
(doc. MUDr. Ľubica Kováčiková, PhD.)
A firm believer in holistic healing, Dr. Kováčiková won our trust with ease. Even years after leaving her ICU, we still turn to her for advice on supporting Emanuela's needs beyond pharmaceutical and traditional medical treatments.
ICU hospitalization delays sensory-motor development and affects a child's mental state and communication skills. Basal stimulation is invaluable in critical care, particularly when a child is sedated and unable to develop naturally.
(Doc. MUDr. Ľubica Kováčiková, PhD.)
Basal stimulation is now an accredited practice by the Ministry of Health, with specialized training available for nurses, doctors, physiotherapists, occupational therapists, clinical speech therapists, psychologists, and other healthcare professionals.

Involving Parents
That first touch - when my finger hesitantly crossed my baby's tiny hand - soon led to gentle massages of my girl's arms and legs, attempting to stimulate the muscles she couldn't use while lying still in her bed.
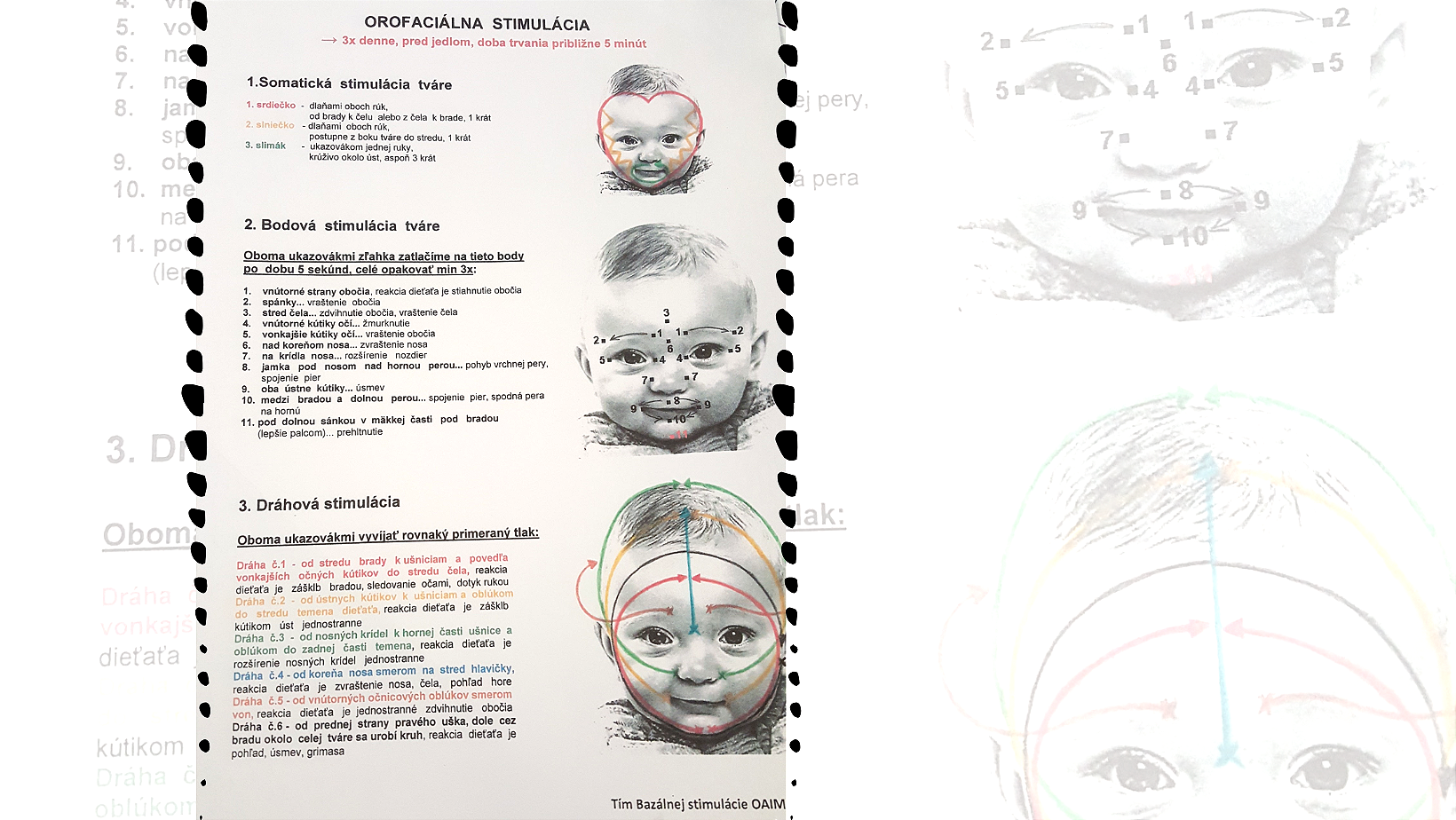
Months later, after her second open-heart surgery caused permanent vocal cord damage, sucking on a pacifier triggered her gag reflex. Worse, feeding became a struggle - bottles of milk made her gag and vomit. Before resorting to a long-term feeding tube placement (jejunostomy), someone suggested basal stimulation.
We tried specially designed facial strokes to activate the muscles needed for sucking and swallowing. Routine, repetitive movements - stroking her cheek, massaging around her mouth - aimed to reawaken her lost instincts. Sticking to the schedule wasn't easy. Between medical procedures, check-ups, and follow-ups, incorporating alternative therapies sometimes felt nearly impossible. But we did our best, knowing this wasn't a miracle cure, but just another layer of support for our daughter's recovery. In the end, she had to have a jejunostomy placed, but even so, we continued with the basal stimulation at home. Against a few doctors' expectations of her needing the tube for years, I weaned my baby off tube feeding before her first birthday.
Basal stimulation, as I came to understand it, was about more than rehabilitation. It was about the power of touch, presence, and involvement in my child's care.
Parental involvement fosters cooperation between nurses and families, eases communication barriers and tensions that arise from the severity of the situation, as well as helps parents feel empowered in their child's recovery.
(doc. MUDr. Ľubica Kováčiková, PhD.)
I can attest to that! During those long months of Emanuela's hospitalization, basal stimulation gave me a purpose. It allowed me to feel useful and connected to my bedridden baby. In a situation where I had no control over what was happening or what would come next, and feeling helpless due to my lack of medical knowledge, the prescribed time and activities I was taught to do with my child became an anchor. I'm certain that by helping myself in this way, I was also helping my baby girl.
Inviting parents to participate - whether through direct caregiving, discussions about their child's preferences, or even by bringing familiar personal items - helps them regain a sense of peace and purpose during this critical life situation. The basal stimulation approach, through the staff's demonstrated interest in the child, reinforces the message that the child is in good hands, and safe even when the parent is not there. This reassurance improves parental mood, sleep, and reduces feelings of helplessness and anxiety. In end-of-life care, the basal stimulation principles provide comfort to the child and their family, helping them navigate the terminal phase in the most humane way possible while ensuring the highest quality of experience for the child in their final moments.
(doc. MUDr. Ľubica Kováčiková, PhD.)
In practice, this means surrounding the child with pictures and familiar objects, pleasant sounds, and even scents. I remember how these small but meaningful comforts were implemented in our case.

In 2018, during our early days of navigating hospital life, I often arrived at the ICU to find Emanuela arranged in ways that surprised me. One time, while she was still heavily sedated, battling withdrawal symptoms as the medications wore off, a nurse placed earphones near her ears and played Baby Mozart to help her relax.
These moments, seemingly small, made a world of difference.
In 2021, when Emanuela was hospitalized in the ICU after her Fontan surgery at the University Hospital of Leuven (Belgium), she was no longer a baby. This meant she was acutely aware of her surroundings. It was one of the COVID years, and strict visitation limits meant leaving her alone in an unfamiliar place, terrified of masked and uniformed staff constantly working around her. It was a horror for both of us. Desperate to reassure her that we would always come back, I left my sweater by her side - one I had worn for days, fragrant with my scent. My skeptical self was stunned when I saw her snuggling into it each time we returned.

Basal stimulation principles emphasize familiarity: older children should use their own toiletries whenever possible for bathing and skincare. If they cannot brush their teeth, they should have familiar liquids or flavors to clean their mouth. During that same ICU stay, I learned about lemon swabs - simple yet effective relief for the raw, dry throat left after intubation. Anyone who has been intubated knows the pain and discomfort. Swirling a lemon swab around the mouth, teeth, and gums provides much-needed relief.
Lemon swabs were a bit hit after her third open-heart surgery! (August 2021)
However, integrating all of this into care requires parental involvement. When done in sync, it doesn't just improve the hospitalized child's well-being - it benefits the entire family.
Medical Disclaimer
This article is for informational or educational purposes only. It does not substitute professional medical advice, diagnosis or treatment. Always seek the advice of a physician or other qualified health provider.
*Sources: Quotes taken from the Institute of Basal Stimulation (Czech Republic) website and from Heart is Life [Srdce je život] – Journal of the Children's Cardiac Center Foundation, 1/2025 (Slovakia).